Combining appointment lifecycle and revenue acceleration solutions into one, integrated platform.
Vyne Dental accelerates the conversion of production to collections with a robust, intelligent exchange which automates electronic transmissions of clean claims, analyzed attachments, eligibilities, payments, patient communications, integrated forms, and secure messaging.






Providers
A solution that simplifies claims processing, attachments, and secure messaging is essential for your practice to run smoothly.
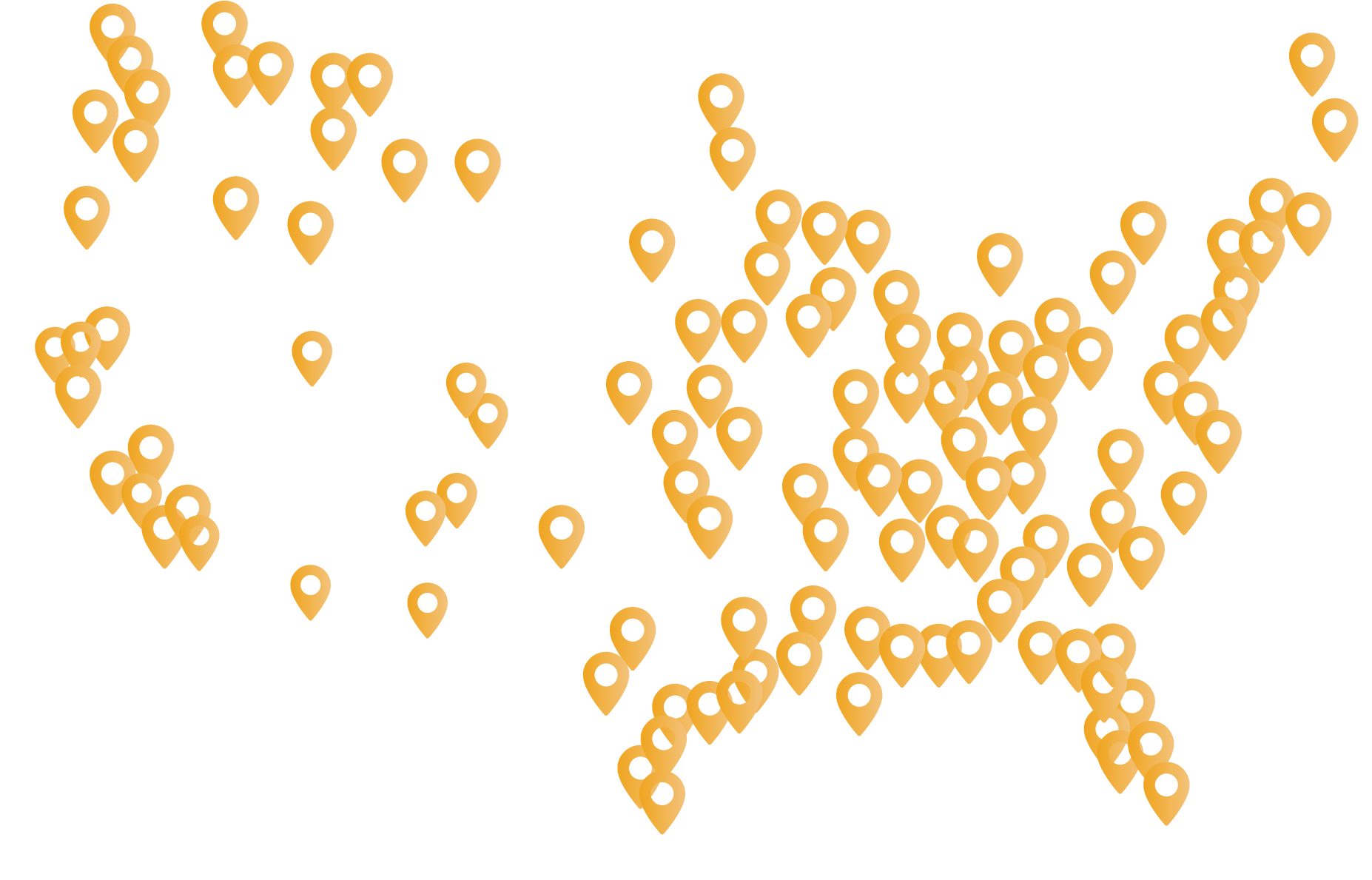
Trusted by over 84,000 successful dental offices nationwide.

Payers
Vyne Dental’s® unified end-to-end electronic platform promotes efficient transactions between payers and providers. We serve insurance companies, dental plans, self-insured employers, and third-party administrators by enhancing dental claims and billing processes through electronic information exchange.
Over 800 connections and growing.

Partners
Driving growth through strategic collaboration and accelerating your success as a Vyne Industry Partner (VIP).
At Vyne Dental, we redefine partnership dynamics.

Vyne Dental Plans
Vyne Dental Plans empower providers to diversify their patient base, better serve their uninsured and self-pay patients, and accelerate patient retention and case acceptance while boosting the top-line.
Cost-effective plans and treatment options for all patients.


Vyne Trellis® is an end-to-end revenue acceleration platform for your practice that streamlines claims submission and tracking, provides batch and real-time eligibility of benefits, and provides a secure environment for your communications.



















Connect with a practice revenue advisor today to learn how to accelerate revenue in your dental practice.